
What priorities for health and healthcare access do women, trans, and nonbinary people who are lesbian, bi+, or queer (LBQ) in Canada have? What actions can be taken across sectors to address these priorities?
Jump to: About the Project | Research Report | Key Findings | Research Visuals
Project Overview
Building on foundational research and critical intersectional approaches, the aim of the project was to learn more about healthcare access experiences among women, trans, and nonbinary people who are lesbian, bi+, or queer (LBQ) and to amplify their perspectives and priorities when it comes to structural and systemic change across care sectors.
Research Report
What priorities for health and healthcare access do women, trans, and nonbinary people who are lesbian, bi+, or queer (LBQ) in Canada have? What actions can be taken across sectors to address these priorities?
Egale’s research report “Healthcare access experiences and needs among LBQ women, trans, and nonbinary people in Canada: A research report” explores these questions, provides recommendations aimed at particular groups (e.g., educators, healthcare practitioners, policymakers), and issues a call to action for sectors to work together to improve healthcare access for LBQ women, trans, and nonbinary people in Canada.
Key Findings
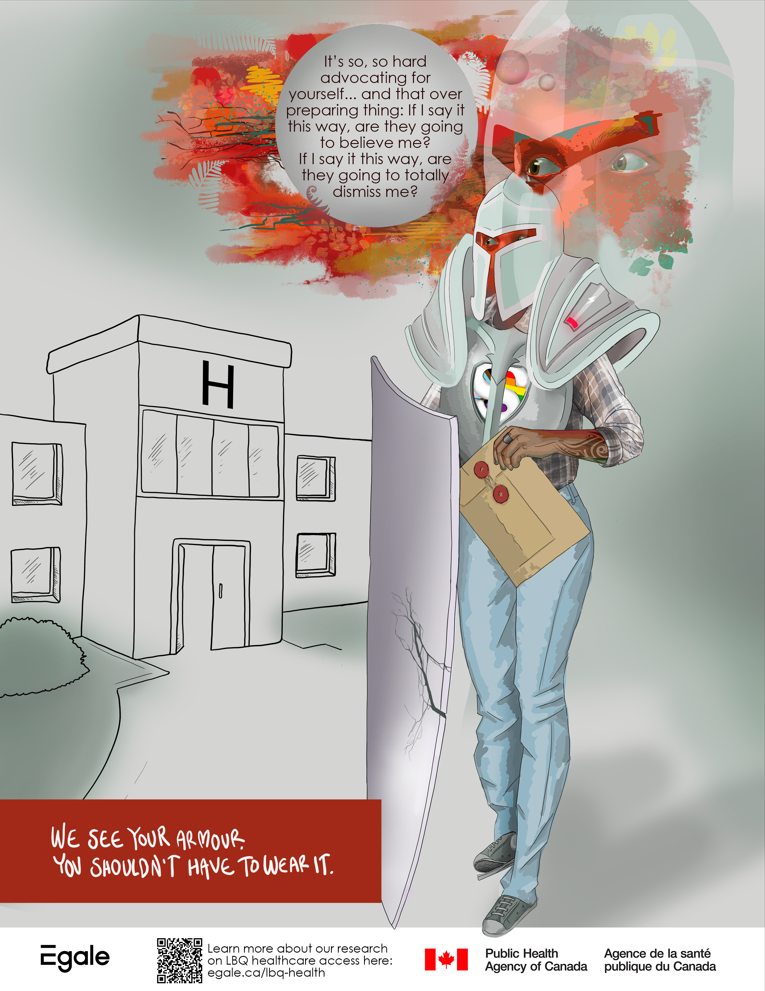
Labour in Accessing Care
A prominent issue highlighted by participants was that of the various forms of labour involved in seeking and accessing care. The efforts and exhaustion in trying to access care often began before initial visits to care providers and had effects on their health and wellbeing beyond the end of medical encounters. Participants described invalidation of their experiential knowledge and felt that the dismissal (medical gaslighting) they experienced was connected to ageism, racism, sexism, and cissexism. Despite these experiences, participants advocated for themselves in various ways.
Accessing Primary Care
Participants discussed their experiences accessing primary care at length, including reflections on finding and interacting with primary care physicians, cost-related barriers, and the use of emergency room care. Participants shared how impeded access to primary care affected their health and wellbeing, options they would like to see, and specific practices they used to try to cover care gaps. They reflected on how their intersecting social locations fundamentally shaped their primary care experiences, and on the systemic changes needed to increase access to competent, affirming, and affordable healthcare.
Sexual and Reproductive Healthcare
Participants sought sexual and reproductive healthcare for a multitude of reasons, including testing, reproductive planning and fertility options, and birth control options and issues. Participants experienced various barriers and challenges in receiving the care they desired such as cost-related barriers, medical paternalism, biphobia, and fatphobia. Nearly all participants shared a negative experience relating to their efforts to have their sexual and/or reproductive care needs met by healthcare providers. Participants shared experiences of navigating identity disclosure and invalidation, discrimination and dismissal, and stigma and shaming.
Gender-Affirming and Transition-Related Healthcare for Trans and Nonbinary People
Trans and nonbinary (TNB) participants’ experiences of healthcare were not always gender-affirming, and those who sought out transition-related healthcare experienced various challenges and barriers such as travel, out-of-pocket costs, and long wait times. TNB participants were up against a cisheterosexist system, and described feeling anxious, fearful, and stressed about accessing care as a trans or nonbinary person. TNB participants noted the increase in availability of virtual and telecare due to the pandemic, and many (especially those who chronic health conditions) expressed a preference for this type of care.
Mental Healthcare
Key issues highlighted by participants regarding mental healthcare experiences were widespread dismissal of their mental health concerns, inaccessibility of services, and the damaging impacts of mental healthcare rooted in paternalistic, biomedical, and colonial frameworks. One of the most cited issues for participants was not being taken seriously or being dismissed. Inaccessibility and unaffordability of most mental healthcare was a commonly noted access barrier, with multiple participants discussing the high cost of mental healthcare. A lack of responsive and affirming 2SLGBTQI services was another access barrier to mental healthcare.
Complementary & Alternative Medicine and Mutual Aid
Participants shared healthcare experiences characterized by emotional and mental labour, gaslighting, inaccessibility, and lack of affirming care. Participants shared examples of stigmatization, marginalization, and discrimination from providers in various healthcare settings (e.g., primary care, sexual healthcare, reproductive healthcare, transition-related care, and mental healthcare). These structural issues and systemic failures served as “push factors” influencing participants to turn toward complementary and alternative medicine (CAM), community-based care, and mutual aid networks to seek information and healthcare. Since CAM is infrequently covered by insurance, access to these services requires significant out-of-pocket expenses.
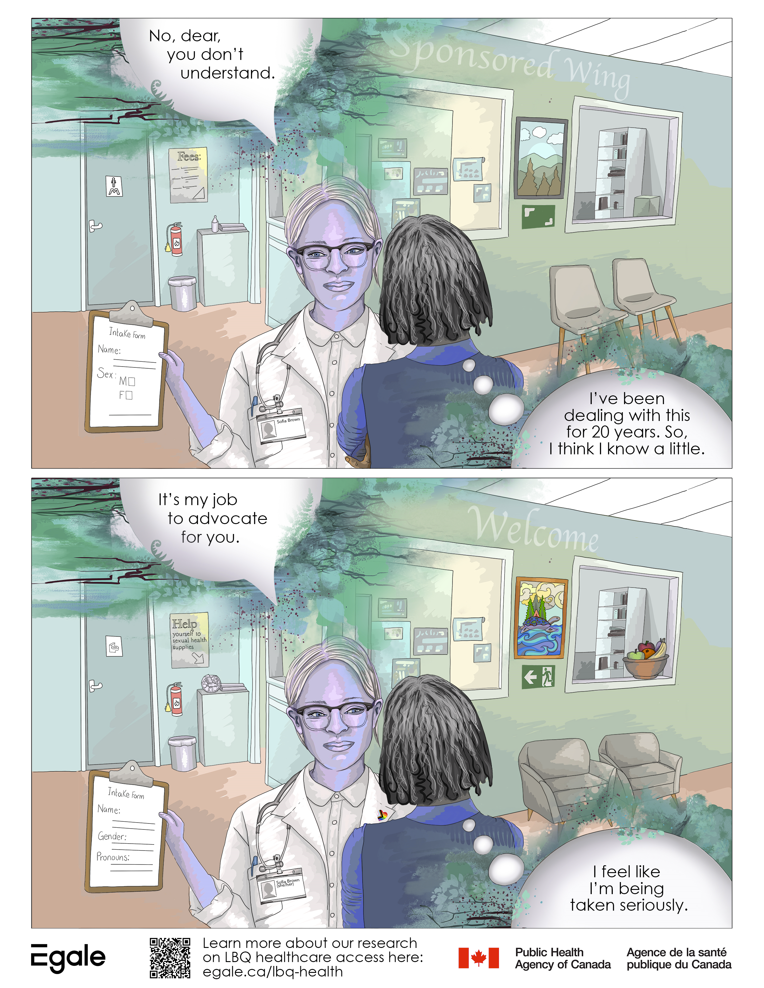
Research Visuals
Egale researchers worked alongside social artist Melanie Schambach to create three research visuals, inspired by participants’ perspectives and experiences of healthcare in Canada. The posters encapsulate project findings and recommendations. These posters can be used freely and displayed in community-based centers, healthcare settings, etc.
All posters are available for download in jpg format (via Google Drive) in the following sizes:
(1) 8.5in x 11in, (2) 18in x 24in, and (3) 24in x 36in.
Armour Poster
12 Differences Poster
Community Poster

Acknowledgments
We thank all contributors and are immensely grateful to each of the participants who so generously shared their time and insights.
This project was funded by the Public Health Agency of Canada Intersectoral Action Fund.
For further questions on this project, please email research@egale.ca.